
Essential Recovery Tips After Surgery Especially for COPD Patients
Imagine waking up after surgery, feeling a wave of relief wash over you as the procedure is complete. But then comes the unexpected tightness in your chest, the struggle to take a deep breath. Surgery, while necessary, can take a toll on your lungs, and for individuals with Chronic Obstructive Pulmonary Disease (COPD), this can be particularly concerning.
The good news is that recovery is a journey, and with proactive measures, you can regain your strength and improve your breathing after surgery. This blog post dives into essential recovery tips and breath training exercise specifically tailored for individuals like you, who are managing COPD alongside surgical recovery.
Why Does Surgery Impact Breathing for COPD Patients?

Several factors contribute to post-surgical breathing difficulties. Anesthesia can temporarily weaken your respiratory muscles, while pain medication might lead to shallower breaths due to discomfort. Additionally, the natural decrease in activity levels during recovery can cause your lungs to become congested, further hindering your breathing.
For individuals with COPD, these factors can exacerbate existing breathing problems. COPD is a progressive lung disease that makes it difficult to breathe. It often involves airway blockage and inflammation, making lung expansion challenging. Post-surgical complications like pneumonia can be more serious for COPD patients due to these underlying conditions.
The Power of Proactive Recovery: Optimizing Your Breath After Surgery
The key to a smooth recovery lies in being proactive about your breathing health. Here are some essential tips to help you breathe easier after surgery:
1. Incentive Spirometry: Your Lung Expansion Partner
An incentive spirometer is a handheld device that helps you take slow, deep breaths, encouraging your lungs to fully expand. This simple tool can significantly reduce the risk of post-surgical complications like pneumonia. Here's how to use it effectively:
- Ask your doctor or nurse for instructions on proper usage.
- Use the incentive spirometer several times a day, following your doctor's prescribed frequency.
- Inhale slowly and deeply through the mouthpiece, raising the piston within the device as much as possible.
- Hold your breath for a few seconds, then exhale slowly.
2. Deep Breathing Techniques: Breathe Deeply, Breathe Easy
Deep breathing techniques like diaphragmatic breathing and pursed-lip breathing can significantly improve your oxygen intake and reduce shortness of breath.
-
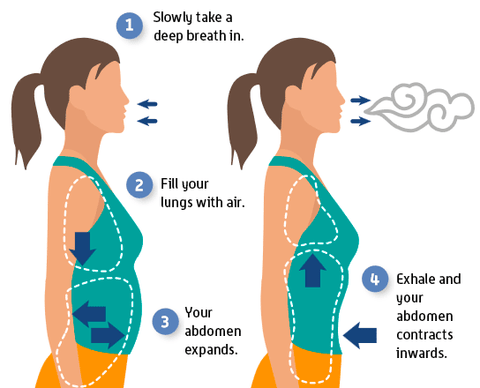
Diaphragmatic Breathing: This technique utilizes your diaphragm, a large muscle below your lungs, for deeper breaths. Here's how to do it:
- Lie on your back with knees bent and feet flat on the floor, or sit comfortably with good posture.
- Place one hand on your chest and the other on your abdomen.
- As you inhale slowly through your nose, feel your abdomen push outwards against your hand, while your chest remains relatively still.
- Exhale slowly through pursed lips, feeling your abdomen sink inwards.
-
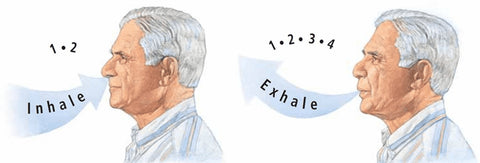
Pursed-Lip Breathing: This technique slows down your breathing rate and helps manage shortness of breath. Here's how to do it:
- Sit or stand comfortably with your shoulders relaxed.
- Inhale slowly through your nose for a count of two.
- Purse your lips as if you're about to blow out a candle.
- Exhale slowly through your pursed lips for a count of four.
Additional Breath Training Techniques:

- Alternate Nostril Breathing (Nadi Shodhana): This technique involves breathing through one nostril at a time, promoting relaxation and improved lung function.
- Close your right nostril with your thumb and inhale slowly through your left nostril.
- Hold your breath for a second (optional), then close your left nostril with your ring finger and exhale slowly through your right nostril.
- Inhale through your right nostril, hold, then exhale through your left nostril. Repeat this cycle for several breaths.
-
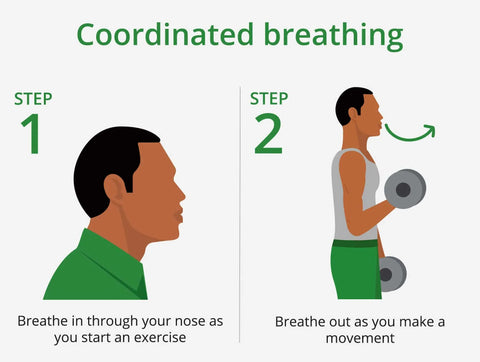
Coordinated Breathing: Coordinated breathing helps synchronize your breath with physical activity, allowing your body to use oxygen more efficiently during exertion. This can benefit activities like exercise, climbing stairs, or even everyday tasks that leave you feeling out of breath. Here's how to perform coordinated breathing:
- Find a comfortable position: Stand tall with relaxed shoulders and good posture. This allows for optimal lung expansion.
- Focus on your breath: Take a few normal breaths to settle in. Notice the natural rhythm of your inhalation and exhalation.
- Inhale through your nose: Breathe in slowly and deeply through your nose for a specific count (e.g., 2 seconds). Feel your belly inflate as your lungs fill with air.
- Exhale through pursed lips: Purse your lips as if you're about to whistle. Exhale slowly and steadily through your pursed lips for a slightly longer count than your inhale (e.g., 3 seconds). Feel your belly contract as you expel air.
By incorporating these deep breathing exercises into your post-surgical routine, you can significantly improve your breathing comfort and promote a smoother recovery. Remember, consistency is key! The more you practice these techniques, the more natural and effective they will become.
3. Pain Management: The Key to Deeper Breaths
Pain can significantly impact your breathing. When you're in discomfort, you tend to take shallower breaths to avoid further pain. This can lead to lung congestion and increased shortness of breath. Here are some tips for managing pain:
- Discuss pain management options with your doctor. Explore non-opioid pain medication alternatives to minimize the risk of shallow breathing.
- Follow your doctor's instructions regarding medication dosage and frequency.
- Consider non-medicinal pain management techniques like applying ice packs or using a heating pad (as approved by your doctor) to target specific areas of discomfort.
4. Positioning and Movement: Find Comfort, Improve Lung Function
Proper positioning can significantly impact your breathing after surgery. Lying flat on your back can compress your lungs, making breathing more difficult. Here are some tips:
- Elevate your head and chest with pillows while sleeping or resting.
- When sitting, ensure good posture with back straight and shoulders relaxed.
- Practice getting out of bed safely with assistance if needed.
- Gradually increase activity levels as tolerated by your doctor. Gentle walks or light stretches can help improve lung function and prevent stiffness.
5. Hydration: Keeping Your Lungs Moist and Clear
Staying hydrated is crucial for optimal lung function. When you're dehydrated, mucus in your airways becomes thicker and stickier, making it harder to clear and further hindering your breathing. Here's how to stay hydrated:
- Aim for eight glasses of water per day, or more if you're sweating heavily.
- Carry a reusable water bottle with you and sip on water throughout the day.
- Consider incorporating hydrating foods like fruits and vegetables into your diet.
6. Nutrition: Building Strength for Recovery
A balanced diet rich in protein is essential for healing and repairing tissues after surgery. Protein helps rebuild muscle, including the muscles responsible for breathing. Here are some tips for post-surgical nutrition:
- Choose lean protein sources like fish, chicken, beans, and lentils.
- Include plenty of fruits and vegetables for essential vitamins and antioxidants.
- Opt for easy-to-digest foods like yogurt, soups, and smoothies, especially in the immediate post-surgical period.
- Consult a registered dietitian for personalized dietary recommendations based on your specific needs and COPD management.
7. Managing COPD Medications: Don't Forget Your Routine
It's crucial to continue taking your COPD medications as prescribed by your doctor, even if your breathing seems to improve initially after surgery. Stopping medications can worsen your COPD symptoms and make breathing difficulties more likely.
8. Communication with Healthcare Providers: Open Dialogue is Key
Open communication with your doctor and nurses is vital for a smooth recovery. Don't hesitate to speak up about any breathing difficulties, increased pain levels, or concerns you might have after surgery. Early intervention can help prevent complications and ensure a more comfortable recovery.
Additional Considerations for COPD Patients
Pre-Operative Planning: Preparing for a Smooth Journey
If you have COPD and are scheduled for surgery, discuss your condition with your doctor beforehand. This might involve:
- Adjusting your COPD medications to optimize your lung function before surgery.
- Scheduling a pulmonary rehabilitation session to learn and practice breathing exercises that can improve your lung function and prepare you for post-surgical recovery.
- Informing your surgeon about your COPD to ensure they are aware of any potential respiratory complications you might face.
Post-Operative Monitoring: Extra Care for Optimal Outcomes
Due to the increased risk of complications, COPD patients might require closer monitoring after surgery. This might involve:
- More frequent breathing assessments to ensure your oxygen levels are stable.
- Chest X-rays to monitor for any signs of pneumonia or other complications.
- Adjustments to your COPD medications based on your post-surgical progress.
Support Groups: Finding Strength in Shared Experiences
Living with COPD can be challenging, and surgery can add another layer of stress. Joining a support group for individuals with COPD can be a valuable resource during your recovery. These groups offer:
- Shared experiences from others who understand the challenges you're facing.
- Information and resources specific to COPD management.
- Emotional support and encouragement throughout your recovery journey.
Understanding Supplemental Oxygen Therapy
For some COPD patients experiencing significant shortness of breath or low blood oxygen levels, their doctor might recommend supplemental oxygen therapy. This involves using a device like a home or portable best oxygen concentrator to deliver a controlled flow of concentrated oxygen.
Benefits of VARON Best Oxygen Concentrators During Recovery
VARON offers a variety of home and portable best oxygen concentrator models to suit diverse needs. These user-friendly devices can provide several benefits during your post-surgical recovery:
- Improved Oxygen Levels: By delivering supplemental oxygen, concentrators can help maintain adequate oxygen levels in your bloodstream, reducing shortness of breath and fatigue.
- Increased Activity Tolerance: With improved oxygenation, you might experience greater stamina and endurance for participating in physical therapy exercises or simply engaging in daily activities with less breathlessness.
- Enhanced Sleep Quality: Low oxygen levels can disrupt sleep. Oxygen therapy can promote better sleep quality, allowing your body to rest and recover more effectively.
Choosing the Right VARON Best Oxygen Concentrator for You
The decision to use supplemental oxygen therapy and the type of concentrator best suited for your needs should be made in consultation with your doctor. However, here's a brief overview of VARON's offerings:
- VARON Home Series (VH-1, VH-2, VH-3): These user-friendly models provide continuous flow oxygen therapy, ideal for individuals who require a steady supply of oxygen at home.
- VARON Portable Series (VL-1, VL-2, VP-1, VP-2): These compact and lightweight options come in both pulse flow and continuous flow, offering greater portability for on-the-go use during your recovery process.
Conclusion: Breathe Easier, Recover Stronger
Recovery after surgery, especially when managing COPD, requires a dedicated and proactive approach. By following these essential tips, prioritizing open communication with your doctor, incorporating personalized strategies into your routine, and considering supplemental oxygen therapy with VARON concentrators, you can optimize your breathing, regain strength, and experience a smoother post-surgical journey. Remember, recovery is a process, and there's no single "one-size-fits-all" solution. Be patient with yourself, celebrate small victories, and don't hesitate to ask for help if you need it.































Leave a comment